How To Cure Sciatica Permanently?
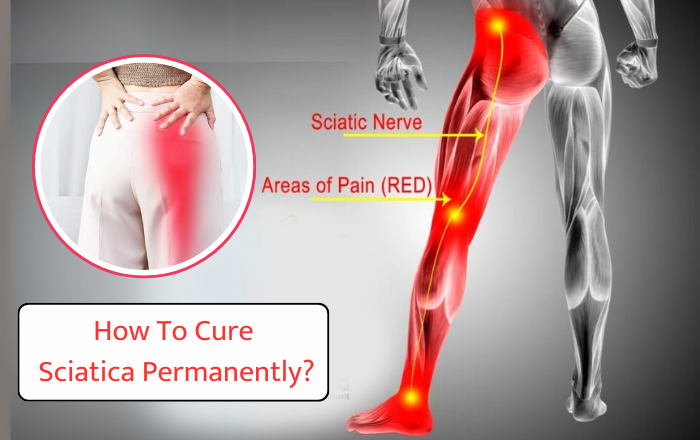
Living with sciatica pain can feel overwhelming. The sharp, shooting pain that starts in your lower back and travels down your leg often disrupts daily activities, leaving you searching for answers. If you’ve been asking, “How can I cure sciatica permanently?” you’re not alone. In this blog, we’ll explore practical ways to address the root cause of sciatica, available treatments, and lifestyle changes that can help you find long-lasting relief. By the end, you’ll have a clear understanding of how to move forward and reclaim a pain-free life. What Is Sciatica? Sciatica is a condition where pain radiates along the path of the sciatic nerve, the longest nerve in the body. It runs from your lower back through your hips, buttocks, and down each leg. Sciatica is not a diagnosis but a symptom of an underlying issue, such as: A herniated disc pressing on the nerve. Spinal stenosis, which narrows the spinal canal. Bone spurs or muscle tightness irritating the nerve. Common symptoms include lower back pain, tingling or numbness in the leg, and difficulty standing or walking. Common Approaches to Treat Sciatica Sciatica pain can be managed through several approaches, but not all provide permanent relief. Let’s take a look at some common methods: Medications: Over-the-counter pain relievers, such as ibuprofen or naproxen, can temporarily reduce inflammation and discomfort. Physical Therapy: Specific exercises can strengthen the muscles around your spine, improve posture, and relieve pressure on the sciatic nerve. Steroid Injections: In severe cases, corticosteroid injections can reduce inflammation and pain for a short time, though they don’t address the root cause. These methods focus on reducing pain but may not provide a permanent solution. Read More Blog – Common Causes of Fractures: Understanding the Risks Can Sciatica Be Cured Permanently? Yes, it is possible to cure sciatica permanently, but this requires treating the root cause. For example: If a herniated disc is causing your pain, treatments such as physiotherapy or surgery may help. If poor posture or muscle imbalances are to blame, correcting these problems can help prevent sciatica from returning. Some people may need surgery, such as a microdiscectomy or laminectomy, if other treatments don’t work. These operations are usually reserved for cases where nerve compression is severe and causing significant problems such as muscle weakness. Non-Surgical Permanent Solutions Many individuals can find lasting relief without surgery. Some effective options include: Physical Therapy: Tailored exercises can strengthen your core muscles, improve flexibility, and relieve nerve pressure. Examples include stretching exercises like the hamstring stretch or yoga poses like the child’s pose. Posture Correction: Sitting, standing, and lifting with proper posture reduces strain on your lower back. Ergonomic chairs and supportive shoes can also help. Spinal Decompression Therapy: A non-invasive technique to relieve pressure on spinal discs, creating space for healing. These methods focus on long-term recovery by addressing the underlying causes of your pain. The Role of a Specialist in Treating Sciatica While many sciatica cases can be managed at home, it’s important to seek medical advice if your symptoms persist or worsen. Specialists like Dr. Parimal Kore, an experienced orthopedic doctor in Magarpatta, can diagnose the exact cause of your sciatica and recommend effective treatment options tailored to your needs. From detailed diagnosis to proven therapies, consulting the right professional can make all the difference in your journey to recovery. Lifestyle Changes for Preventing Sciatica Recurrence Preventing sciatica from coming back is just as important as treating it. Here are some tips: Regular Exercise: Strengthen your core and lower back muscles with low-impact exercises like swimming, walking, or yoga. Healthy Weight: Maintaining a healthy weight reduces pressure on your spine. Ergonomics: Use supportive furniture and proper body mechanics when lifting heavy objects. Stretching Routine: Include daily stretches to keep your back and leg muscles flexible. By adopting these habits, you can significantly lower the risk of future sciatica episodes. FAQs 1. What is the fastest way to cure sciatica permanently? Addressing the root cause, whether through targeted exercises, physical therapy, or surgery in severe cases, is the best way to achieve long-term relief. 2. What are the best exercises to treat sciatica permanently? Exercises like knee-to-chest stretches, cat-cow yoga poses, and hamstring stretches can relieve pressure on the sciatic nerve. 3. Why consult Dr. Parimal Kore for sciatica treatment? Dr. Kore specializes in diagnosing and treating sciatica in Magarpatta. With extensive experience in treating back and nerve conditions, he provides effective solutions to help you regain mobility and comfort.